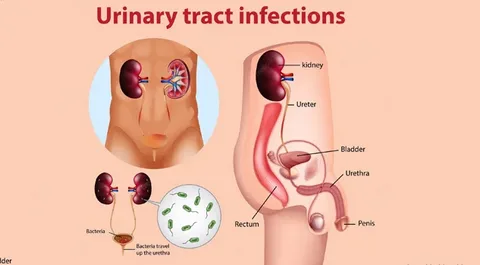
Urinary tract infections (UTIs) remain one of the most common reasons for outpatient visits in St. John and across the globe. Traditional methods of diagnosis, although effective in many cases, often face delays in pathogen identification and antibiotic sensitivity profiling. In recent years, precision molecular diagnostics—specifically CRISPR-based pathogen detection—have revolutionized the speed and accuracy of UTI diagnosis. This article explores the integration of CRISPR technologies into UTI Treatment St. John protocols and how it is reshaping the patient experience and clinical outcomes in the region.
The Diagnostic Challenge in UTI Treatment
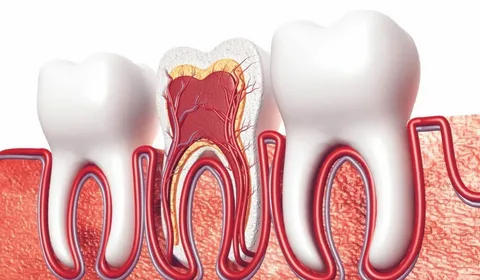
UTIs typically present with symptoms such as burning during urination, frequent urges to urinate, and pelvic pain. Despite these common signs, identifying the underlying cause—especially the bacterial strain responsible—is not always straightforward. In UTI Treatment St. John facilities, traditional diagnostic approaches rely heavily on urine cultures, which can take up to 48 hours or more to deliver conclusive results.
This diagnostic lag has significant clinical implications. Physicians may resort to broad-spectrum antibiotics while awaiting lab confirmation, a practice that contributes to antibiotic resistance—a growing concern in UTI Treatment St. John and globally. Furthermore, culture methods may fail to detect slow-growing or intracellular pathogens, leading to misdiagnosis or recurrent infections.
CRISPR: A Revolutionary Tool in Molecular Diagnostics
Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) were first discovered as part of bacterial immune systems. The gene-editing potential of CRISPR-Cas systems has been widely publicized, particularly in the field of genetics. However, the application of CRISPR for diagnostic purposes—such as SHERLOCK (Specific High Sensitivity Enzymatic Reporter unLOCKing) and DETECTR (DNA Endonuclease Targeted CRISPR Trans Reporter)—has become a major breakthrough.
These systems can rapidly identify bacterial, viral, and even fungal DNA in patient samples with high specificity and sensitivity. CRISPR diagnostics typically utilize guide RNAs to detect unique genetic sequences from pathogens, activating a fluorescent signal when a match is found. In the context of UTI Treatment St. John, this means clinicians can now diagnose the infection within 30 to 60 minutes—offering real-time clinical decision support.
CRISPR-Based Testing in UTI Treatment St. John Clinics
Several progressive clinics and urology specialists in St. John have started integrating CRISPR diagnostics into their UTI Treatment St. John workflow. These clinics benefit from the ability to:
- Identify the exact bacterial strain causing the infection.
- Detect antibiotic resistance genes in the same test.
- Reduce empirical antibiotic prescriptions.
- Improve patient satisfaction by shortening the time to diagnosis.
For instance, women with recurrent UTIs—a group that comprises a significant portion of UTI Treatment St. John cases—often undergo repeated rounds of antibiotics based on symptoms alone. CRISPR allows for more precise targeting, decreasing the recurrence rate.
The Power of Rapid Detection
Traditional urine culture methods detect growth over a two-day period, requiring incubators and skilled technicians. In contrast, CRISPR-based diagnostics, once optimized, are user-friendly and can be implemented even in point-of-care settings.
In a UTI Treatment St. John scenario, a patient arriving with acute symptoms can now provide a urine sample, and within the hour, the clinician may know:
- The species involved (e.g., E. coli, Klebsiella, Proteus).
- The presence of genes associated with resistance to common antibiotics such as ciprofloxacin or trimethoprim-sulfamethoxazole.
This level of precision was not previously available in routine UTI Treatment St. John assessments.
Addressing Recurrent and Complicated Infections
One of the most frustrating experiences for both patients and clinicians is the case of recurrent UTIs. These often stem from incomplete eradication of the original bacteria, misidentification, or colonization by multiple pathogens. In UTI Treatment St. John, recurrent UTI patients frequently undergo invasive testing and long-term prophylactic antibiotics.
CRISPR technology mitigates this issue by allowing for multiplexed detection. That is, a single test can simultaneously screen for multiple pathogens and resistance markers. This prevents oversight of co-infections and ensures that antibiotics are tailored to the patient’s specific microbial landscape.
How CRISPR Enhances Stewardship in UTI Treatment St. John
Antibiotic stewardship is a major public health focus in the U.S., including in the St. John area. Overprescription contributes to resistant superbugs, which complicate UTI treatment efforts and increase healthcare costs. By leveraging CRISPR diagnostics, clinicians in UTI Treatment St. John programs are better equipped to:
- Minimize unnecessary prescriptions.
- Match antibiotics to susceptibility profiles with confidence.
- Monitor resistance trends in real time.
In several pilot programs across Indiana, including select St. John clinics, the integration of CRISPR diagnostics has led to a 25–40% reduction in broad-spectrum antibiotic use in UTI cases—an impressive metric for public health advocates.
Real-World Case Studies from St. John
Let’s consider a few anonymized real-world examples to demonstrate the impact of CRISPR-based diagnostics in UTI Treatment St. John:
Case 1: Elderly Female with Frequent Recurrences
An 80-year-old woman with type 2 diabetes presented with her fifth UTI in six months. Traditional cultures repeatedly showed E. coli, but antibiotic courses only provided temporary relief. A CRISPR-based test revealed co-infection with Enterococcus faecalis and presence of an ESBL gene (Extended Spectrum Beta-Lactamase). Treatment was adjusted accordingly, and her symptoms resolved completely.
Case 2: Young Athlete with Atypical Symptoms
A 24-year-old male athlete reported pelvic discomfort and occasional urgency without fever. Urine culture was negative, but CRISPR testing detected Mycoplasma genitalium, a fastidious organism missed by culture. A course of doxycycline resolved the symptoms. This diagnosis would have been impossible under standard UTI Treatment St. John testing paradigms.
Limitations and Ongoing Research
Despite its promise, CRISPR-based diagnostics are not without limitations. These include:
- Cost and availability: Currently more expensive than culture.
- Regulatory approval: Only some tests are FDA-approved for clinical use.
- Training requirements: Clinics need to adapt workflows and train staff.
Still, research is ongoing to develop fully automated, affordable CRISPR kits that can integrate seamlessly into primary care and urology practices in UTI Treatment St. John centers.
Integration with Electronic Health Records
Another advantage of CRISPR-based systems is their compatibility with cloud-based health platforms. Once a test is run, results can be uploaded to a patient’s EHR in real time. This allows UTI Treatment St. John physicians to remotely review, prescribe, or adjust therapy almost instantaneously, improving accessibility for patients in rural or underserved areas.
The Future of UTI Treatment St. John with CRISPR
The future of UTI Treatment St. John is moving swiftly toward personalized, precision medicine. With CRISPR-based diagnostics becoming faster and more affordable, the model of treating based on symptoms and delayed cultures is becoming obsolete.
We can expect the following developments in the next five years:
- Widespread use of handheld CRISPR diagnostic devices.
- Integration of resistance trend dashboards for local communities.
- Enhanced monitoring of recurrent UTI patients through molecular profiling.
CRISPR not only empowers clinicians but also restores confidence in patients by delivering accurate answers and targeted care. As UTI Treatment St. John clinics continue to adopt this cutting-edge technology, the standard of care for urinary infections is being irrevocably elevated.
FAQs
Q1: How does CRISPR testing improve UTI Treatment St. John outcomes?
A1: CRISPR testing identifies the specific pathogen and its resistance genes within an hour, allowing physicians in UTI Treatment St. John to prescribe the most effective, targeted antibiotics. This leads to faster recovery, fewer recurrences, and reduced antibiotic misuse.
Q2: Is CRISPR testing available in all St. John clinics?
A2: Not yet. While some advanced urology and infectious disease clinics in St. John have adopted CRISPR-based diagnostics, others are in the process of acquiring the technology. The cost and regulatory approvals are still being navigated in broader UTI Treatment St. John adoption.
Q3: Can CRISPR detect multiple pathogens in one test?
A3: Yes. One of the key advantages of CRISPR diagnostics in UTI Treatment St. John is its multiplex capability. It can identify co-infections and resistance genes in a single assay, which is particularly useful in complex or recurrent UTI cases.